Cystic Fibrosis Symptoms
Cystic fibrosis is a multi-system progressive condition, so people with this condition can experience a variety of symptoms. Symptoms usually develop within the first year of life but may not appear until your teenage years or adulthood. Cystic fibrosis signs and symptoms can vary with age, with disease severity and with the disease-causing mutations you have.
People with cystic fibrosis may have salty-tasting sweat caused by a higher than normal level of salt.6
In your lungs, thick and sticky mucus can clog your airways and trap bacteria. This causes respiratory symptoms such as:6
- Persistent (chronic) cough with thick mucus
- Wheezing and shortness of breath (breathlessness)
- Frequent lung infections which may include pneumonia
- Inflamed nasal passages or a stuffy nose
- Recurrent sinus infections (known as sinusitis)
The pancreas is an organ that makes enzymes that help digest your food. Thick, sticky mucus can block the tubes that carry digestive enzymes from your pancreas to your small intestine and cause digestive symptoms such as:6
- Foul-smelling, greasy stools
- Poor weight gain and poor growth
- Meconium ileus – an intestinal (bowel) blockage in a newborn baby
- Chronic or severe constipation
Atypical cystic fibrosis is a milder form of the disorder. Instead of having classic symptoms, you might only have mild dysfuntion in one organ system and you may have normal sweat chloride levels. Symptoms can fluctuate over time and may not begin until adolescence or adulthood.7
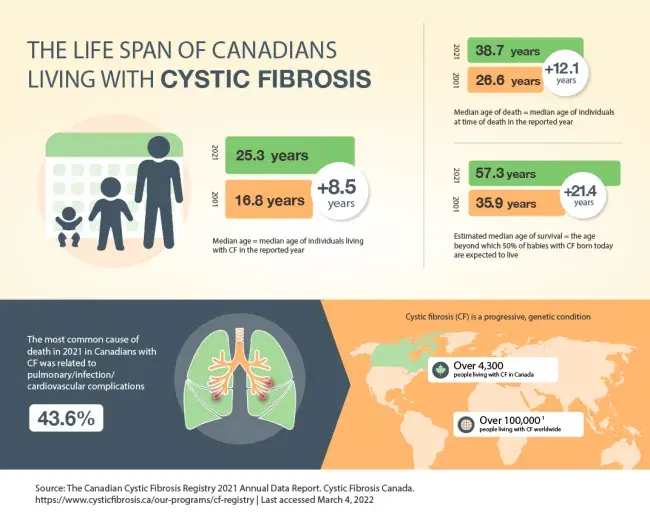
Cystic Fibrosis Life Expectancy
Cystic Fibrosis Complications
Complications of cystic fibrosis will depend on the affected organs and the severity of the disease.
Possible complications are:
- Cystic fibrosis bronchiectasis (CF bronchiectasis) is a chronic lung condition with abnormal widening and scarring of the bronchial tubes that is caused by cystic fibrosis6
- Chronic infections in the lungs and sinuses can cause sinus infections, bronchitis (inflammation of the lining of your bronchial tubes) or pneumonia6
- Pseudomonas aeruginosa bacteria is a major cause of lung infections in people with cystic fibrosis.8 It’s thought that people get Pseudomonas aeruginosa infections from the environment and from other people who are infected with the bacteria (called cross-infection).8 Typically, Pseudomonas aeruginosa doesn’t infect healthy people. However in CF, cross-infection poses a particular threat. To minimize risk of cross-infection people with cystic fibrosis aren’t encouraged to socialize with each other. Guidelines9 recommend maintaining a distance of at least 6 feet (2 metres) apart
- Mycobacterium abscessus (M. abscessus) is the most common strain of non-tuberculous mycobacteria (NTM), a family of common organisms found in water and soil that can cause lung infections in people with cystic fibrosis10
- Other bugs that can be passed on through cross-infection are Burkholderia cepacia complex (B cepacia) and the fungus Aspergillus fumigatus 10
- Acute exacerbations (or flare ups) when respiratory symptoms become worse6
- Respiratory failure6
- Cystic fibrosis-related diabetes (CFRD) is a unique type of diabetes found in people with CF6
- Liver disease6
- Distal intestinal obstruction syndrome (DIOS) is a partial or complete blockage of the intestines by thickened stool6
- Infertility in men (due to an abnormality/absence of the vas deferens) and decreased fertility in women6
- Osteoporosis – thinning of the bones to the point of brittleness6
- Nasal polyps are soft, fleshy growths in the nose caused by chronic inflammation in the nasal lining6
- Mental health problems such as depression and anxiety6