Cystic Fibrosis Diagnosis
In 2021 in Canada, 60.5% of individuals with CF were diagnosed before the age of one year, and 73.1% were diagnosed by the age of two years. Only 8.1% of all individuals diagnosed in 2021 were 18 years of age or older.5
In 2021, 68.4% of new CF diagnoses in Canada were identified through newborn screening (NBS).5 Newborn screening programs in all provinces across Canada screen for cystic fibrosis and a number of other health conditions. Shortly after birth, a small blood sample is taken from the baby’s heel (the heel prick blood test). To screen for cystic fibrosis, the blood sample is checked for a chemical made by the pancreas called immunoreactive trypsinogen (IRT). IRT is normally found in small levels in the body. If the initial IRT screen is high or positive, more testing is needed to determine if the infant has cystic fibrosis or not. These tests may include a sweat test or a genetic test.
A cystic fibrosis sweat test (also known as a sweat chloride test) is used to diagnose CF in infants, children and adults. In the test a small amount of sweat is collected from the surface of your skin and the chloride or salt content is measured. People with CF may have very salty sweat. For a person who has CF, the sweat test results typically confirm the diagnosis by showing a high chloride level.
Genetic testing is used to determine the exact gene mutation. More than 2,000 different CFTR gene mutations have been identified.11 One of the most common is the delta F508 mutation.11 The specific mutations and combination of genes you have is known as your genotype. Your genotype will dictate the symptoms you have and the treatments you take.
In children who are not diagnosed by newborn screening, most are diagnosed with cystic fibrosis once they start to show symptoms. Common symptoms in children include chronic coughing, not gaining weight as well as expected, and abnormal bowel movements.
Babies may be diagnosed with CF at or shortly after birth due to meconium ileus. In this condition the baby’s gut becomes blocked with meconium – a black or dark green, tarry substance that is made in all babies’ intestines before birth and usually comes out in a baby’s first poop. Babies born with this problem may need urgent surgery to remove the blockage.
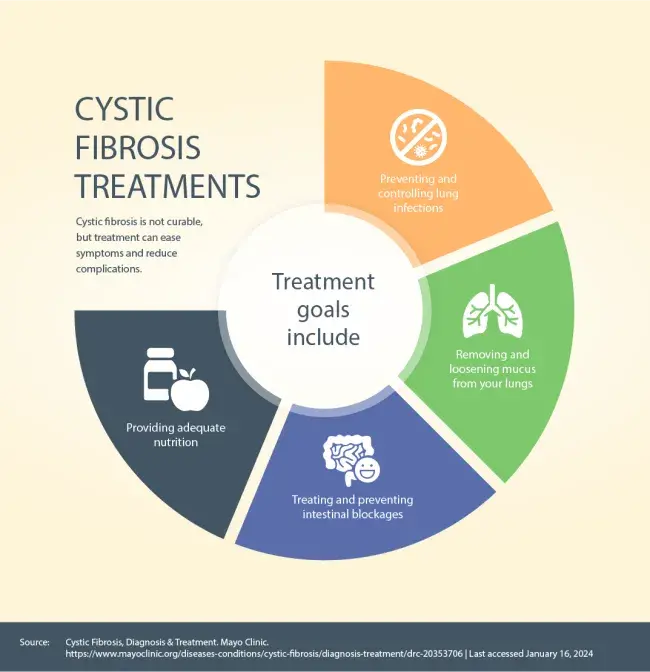
Cystic fibrosis is not curable, but treatment can ease symptoms and reduce complications. Treatment goals include:12
Non-Medication Based Treatments
Airway Clearance
Airway clearance is essential in cystic fibrosis care. Airway clearance therapy (ACT) uses non-invasive techniques to help loosen mucus or sputum so it can be cleared from your airways by coughing or huffing.
There are many different airway clearance techniques. It’s important to speak with your health care provider to find the type and frequency of treatment that’s best for you or your child.
Chest physical therapy or physiotherapy (CPT), also known as postural drainage and percussion (PD&P) is performed by your health care provider or care giver.13 You’re placed in several different postures or positions to help drain mucus from different parts of your lungs using gravity. Percussion or clapping on your chest wall is done by your care provider to help move the mucus into your larger airways so it can be coughed out. Most babies and toddlers with cystic fibrosis use physiotherapy to keep the lungs clear of mucus.
Self-administered airway clearance techniques include:
Autogenic drainage (AD):13
- Autogenic drainage uses a cycle of controlled breathing exercises to clear different levels of your lung. This technique moves mucus from the small airways to the medium-sized airways and then to the larger airways to be coughed out. Assisted autogenic drainage is used in babies.
Active cycle of breathing techniques (ACBT):13
- ACBT combines breathing control, deep breathing (thoracic expansion) exercise and huffing (forced expiration technique) performed in a cycle.
Oscillating positive expiratory pressure (OPEP) therapy:13
- An OPEP device is a handheld device that combines positive expiratory pressure (PEP) with oscillations (or vibrations) to help clear secretions from your airways. As you exhale through the mouthpiece, positive pressure holds the airways open and allows air to get behind the mucus. Oscillations help to thin, loosen and move the mucus to the larger airways of your lungs where it can be coughed out.
Positive expiratory pressure (PEP) therapy:13
- A PEP device is a handheld device that creates positive pressure when you exhale through the device’s mask or mouthpiece. The positive pressure holds open the airways in your lungs, allowing air to get behind the mucus and loosen it so you can cough it out.
High frequency chest wall oscillation (HFCWO) therapy:13
- In this technique external chest wall oscillations are applied to your torso using a fitted vest. The vest produces vibrations to help loosen and thin mucus and separate it from airway walls so it can be coughed up.
Intrapulmonary percussive ventilation (IPV):13
- This technique uses a pneumatic device to deliver short bursts of air into your lungs at a high rate. These percussive bursts of air are delivered during inhalation and exhalation and help to loosen and mobilize secretions to your upper airways where they can be coughed out.
Exercise
Physical activity plays an important role in maintaining the health and well-being of people with cystic fibrosis. Exercise may help to improve health-related quality of life.14 You should speak with your health care provider about the type and intensity of exercise suitable for you.
Nutrition and Diet
In most people with cystic fibrosis, the small channels that carry enzymes from the pancreas to the small intestine become blocked with mucus, preventing food from being digested and absorbed (this is called pancreatic insufficiency). Babies, children and adults with CF take pancreatic enzyme supplements to help digest food. You may also need a much higher number of calories each day to maintain a healthy weight.
Mental Health
Living with cystic fibrosis or caring for someone with CF can take a toll on your emotional well-being. Maintaining physical distance from others with CF to avoid cross infection can lead to feelings of isolation. It’s important to reach out to your CF care team to discuss resources that are available to help you.
Organ Transplants
Transplantation may be the next step for a person with advanced CF to extend and improve quality of life. Lung transplants are most common, as the lungs are most affected by cystic fibrosis. However, some people may need liver and other organs transplanted. Transplant is not a cure for CF.