Bronchiectasis is a chronic, progressive lung condition affecting infants, children and adults. While the global prevalence of bronchiectasis is not accurately known,1 there is a growing awareness of the disease.2
About Bronchiectasis
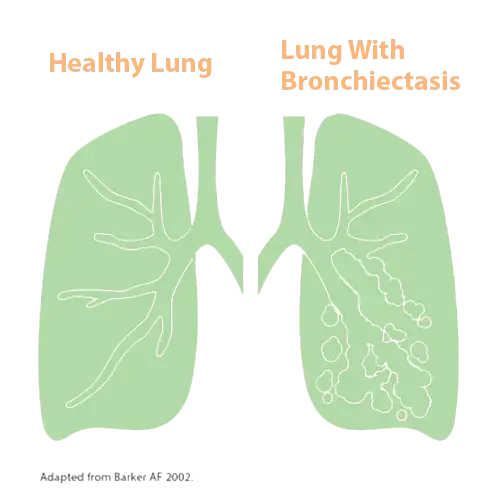
Bronchiectasis is characterized by permanently widened or dilated airways (know as bronchi) with thick walls and scarring. Your airways produce mucus (also called sputum) to help trap and remove germs and particles that enter your lungs. Tiny hair-like structures called cilia help move mucus out of your airways up to your throat to prevent infection. Bronchiectasis damages your cilia, so your airways can’t clear themselves properly. When this happens, mucus builds up in pockets in the widened airways and attracts bacteria – leading to a chronic cycle of lung infections and inflammation, and further damage to your airways.
There’s no cure for bronchiectasis – but treatment can help you manage your condition. Most people diagnosed with bronchiectasis have a normal life expectancy.3
Types of Bronchiectasis
Bronchiectasis affects people of all ages. You can be born with the condition (called congenital bronchiectasis) or you can acquire it later in childhood or as an adult as a result of another condition or factor that damages your lungs or increases your risk of lung infections (this is known as acquired bronchiectasis).5 Bronchiectasis isn’t contagious.6
The likelihood or risk of getting bronchiectasis increases with age.7 Most people newly diagnosed with bronchiectasis are adults.8 It’s not a common condition in babies or children, but they can be affected.8
Bronchiectasis may affect many areas of your lung (diffuse) or appear in only one or two areas of your lungs (focal).9
There are two kinds of bronchiectasis – bronchiectasis that is unrelated to cystic fibrosis (commonly called non-CF bronchiectasis) and cystic fibrosis bronchiectasis (CF bronchiectasis).10
|

|
References
1.International Respiratory Coalition. Lung Facts - Diseases - Bronchiectasis. https://international-respiratory-coalition.org/diseases/bronchiectasis/ (Last accessed January 17, 2024).
2. Martina Contarini. Bronchiectasis: a case-based approach to investigation and management. European Respiratory Review 2018;27:180016. https://err.ersjournals.com/content/27/149/180016.
3. Living with Bronchiectasis. British Lung Foundation 2017;BK33 Version 1. https://www.blf.org.uk/sites/default/files/BK33_Bronchiectasis_v1_2017_PDFdownload.pdf (Last accessed January 17, 2024).
4. Alan F Barker. Bronchiectasis. The New England Journal of Medicine 2002.;346:1383-1393. https://www.nejm.org/doi/full/10.1056/NEJMra012519.
5. Bronchiectasis. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/bronchiectasis (Last accessed January 17, 2024).
6. Bronchiectasis Frequently Asked Questions (FAQs). Bronchiectasis and NTM 360°. https://www.bronchiectasisandntminitiative.org/Learn-More/I-am-a-Patient-or-Caregiver/Bronchiectasis-FAQs (Last accessed February 23, 2024).
7. Doreen Addrizzo-Harris, et al. Living Well With Bronchiectasis Patient Information Guide. CHEST Foundation 2017. https://foundation.chestnet.org/wp-content/uploads/2020/05/Bronchiectasis-Living-Well.pdf (Last accessed January 17, 2024).
8. Bronchiectasis in children. British Lung Foundation. https://www.blf.org.uk/support-for-you/bronchiectasis-in-children/what-is-it (Last accessed January 17, 2024).
9. Galit Livnat, et al. Non-cystic fibrosis bronchiectasis: review and recent advances. F1000 Medicine Reports 2009;1:67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2948306/.
10. Jaafer Saadi Imam, Alexander G Duarte. Non-CF bronchiectasis: Orphan disease no longer. Respiratory Medicine. 2020;166:105940. https://www.sciencedirect.com/science/article/pii/S0954611120300809
11. Adam T Hill, et al. British Thoracic Society Guideline for Bronchiectasis in Adults. Thorax 2019;74(1):1-69. http://dx.doi.org/10.1136/thoraxjnl-2018-212463.
12. Bronchiectasis in children. British Lung Foundation. https://www.blf.org.uk/support-for-you/bronchiectasis-in-children/what-is-it (Last accessed January 17, 2024).
13. MP Murray, et al. Sputum colour: a useful clinical tool in non-cystic fibrosis bronchiectasis. European Respiratory Journal 2009;34(2):361-364. https://erj.ersjournals.com/content/34/2/361.
14. How is bronchiectasis diagnosed? British Lung Foundation. https://www.blf.org.uk/support-for-you/bronchiectasis/diagnosis (Last accessed January 17, 2024).
15. Severity assessment. EMBARC The European Bronchiectasis Registry. https://www.bronchiectasis.eu/severity-assessment (Last accessed January 17, 2024).
16. Bronchiectasis: Symptoms. National Jewish Health. https://www.nationaljewish.org/conditions/bronchiectasis/bronchiectasis-overview/symptoms (Last accessed January 17, 2024).
17. What is the treatment for bronchiectasis? British Lung Foundation. https://www.blf.org.uk/support-for-you/bronchiectasis/treatment (Last accessed January 17, 2024).
18. Annemarie L Lee, et al. Airway-Clearance Techniques in Children and Adolescents with Chronic Suppurative Lung Disease and Bronchiectasis. Frontiers in Pediatrics 2017;5(2):1-8. https://doi.org/10.3389/fped.2017.00002.
19. Eva Polverino, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. European Respiratory Journal 2017;50:1700629. DOI: 10.1183/13993003.00629-2017. https://erj.ersjournals.com/content/50/3/1700629.
20. Bronchiectasis Toolbox. https://bronchiectasis.com.au/bronchiectasis/living-with-bronchiectasis/nutrition (Last accessed January 17, 2024).