PURPOSE
MDIs are the most common type of inhaler in North America and an important device option for many respiratory patients. The addition of a spacer has been shown to:
- Overcome coordination issues
- Improve lung deposition
- Reduce side effects due to oropharyngeal deposition
The objective of this assessment was to evaluate the general impact of treating patients with a MDI/Spacer delivery system rather than MDI alone, using literature search and scenario modeling.
METHODS
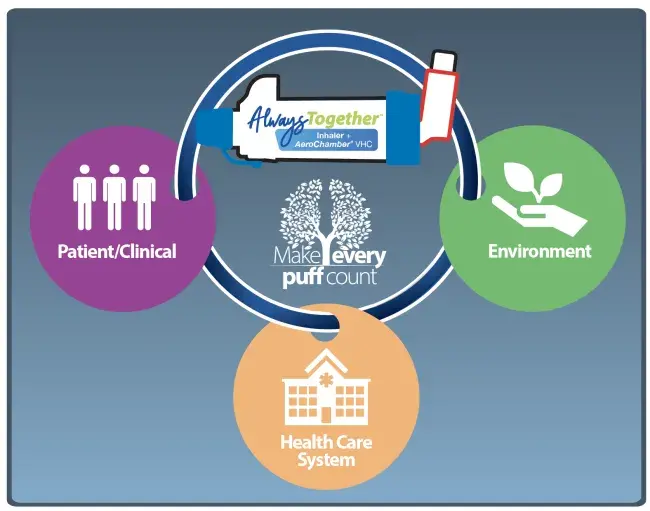
A literature search was undertaken to identify published pharmacokinetic (PK) studies in which lung delivery data was generated directly comparing MDI alone and MDI/AeroChamber* brand of spacer systems, the aim being to assess the relationship and determine the average ratio. Based upon the observed relationship, modelled impact assessments were generated for both reliever and controller MDIs in terms of:
- patient/clinical
- health care system
- environment
RESULTS
Three published pharmacokinetic (PK) studies were identified using current MDIs, all of which reported direct comparisons between MDI and MDI/Spacer
(AeroChamber Plus* brand) lung delivery.
Focusing on the AUC data, it was observed that the mean MDI alone deliveries to the lungs (as percentage of mean delivery for MDI/Spacer combination) were 35%, 39% and 70%. As such, a grouped average of 48% (or a 2x increase if viewed as MDI to MDI/VHC) was used for the impact assessments.

For Reliever MDIs it was modelled that the potential impact of switching MDI to MDI/Spacer for patient was quicker relief of symptoms, for health care system was up to a 50% saving in the cost of MDIs, and for the environment was up to 50% reduction in carbon emissions.
For Controller MDIs it was modelled that the potential impact of switching MDI to MDI/Spacer for patient was better disease control and management of symptoms plus less ICS related side effects, for health care system was savings due to less step ups in dose and less hospitalizations, and for environment was no change or reduction in carbon emissions if patient was on MART therapy
| Study | MDI | Subjects | Mean Age | Mean Area Under Curve (AUC) for MDI alone / Mean AUC for MDI +AeroChamber* VHC |
|---|---|---|---|---|
| 1 Dorinsky P et al. Relative Bioavailability of Budesonide/Glycopyrrolate/Formoterol Fumarate Metered Dose Inhaler Administered With and Without a Spacer: Results of a Phase I, Randomized, Crossover Trial in Healthy Adults. Clin Ther. 42 (2020),634-648. | Breztri† / Trixeo† (Budesonide, Glycopyrrolate, Formoterol Fumarate) | 56 healthy adults | 29.9 years | 50%, 29%, 27% —> 35% |
| 2 Gillen M et al. Effect of a spacer on total systemic and lung bioavailability in healthy volunteers and in vitro performance of the Symbicort ® (budesonide / formoterol) pressurized metered dose inhaler. Pulmon PharTher. 2018 Oct;52:7-17. | Symbicort† (Budesonide, Formoterol Fumarate) | 50 healthy adults | 42 years | 41%, 37% —> 39% |
| 3 Singh D et al. Effect of AeroChamber Plus on the lung and systemic bioavailability of beclomethasone dipropionate / formoterol pMDI. British Journal of Clinical Pharmacology. 72:6; 932–939. 2011. | Fostair† / Foster†(beclomethasone dipropionate /formoterol) | 12 healthy adults | 29.2 years | 71%, 69% —> 70% |
| 48% grouped average |