Common Treatments
Bronchiectasis is a long-term condition. Early treatment is important to help improve how you feel and to keep your condition well managed. If left untreated, your symptoms may progress causing further damage to the airways in your lungs.16 Treatment goals for bronchiectasis in children and adults are: 5,17 - Treat lung infections
- Clear mucus from your lungs through airway clearance therapy
- Prevent further damage
- Reduce your symptoms
|
|
Airway Clearance
Airway clearance is an important way to manage bronchiectasis in infants, children and adults. Airway clearance therapy (ACT) uses non-invasive techniques to help loosen mucus or sputum so it can be cleared from your airways by coughing or huffing.
There are many different airway clearance techniques. It’s important to speak with your health care provider to find the type and frequency of treatment that’s best for you or your child.
Chest physical therapy or physiotherapy (CPT), also known as postural drainage and percussion (PD&P) is performed by your health care provider or care giver.11,18 You’re placed in several different postures or positions to help drain mucus from different parts of your lungs using gravity. Percussion or clapping on your chest wall is done by your care provider to help move the mucus into your larger airways so it can be coughed out. This technique is suitable for infants and small children who are not yet old enough to cooperate with more active techniques. It’s also an option for those unable to use or too fatigued to use independent techniques.18
Self-administered airway clearance techniques include:
- Autogenic drainage (AD)11,18
Autogenic drainage uses a cycle of controlled breathing exercises to clear different levels of your lung. This technique moves mucus from the small airways to the medium-sized airways and then to the larger airways to be coughed out.
- Active cycle of breathing techniques (ACBT)11,18
Active cycle of breathing techniques combines breathing control, deep breathing (thoracic expansion) exercise and huffing (forced expiration technique) performed in a cycle.
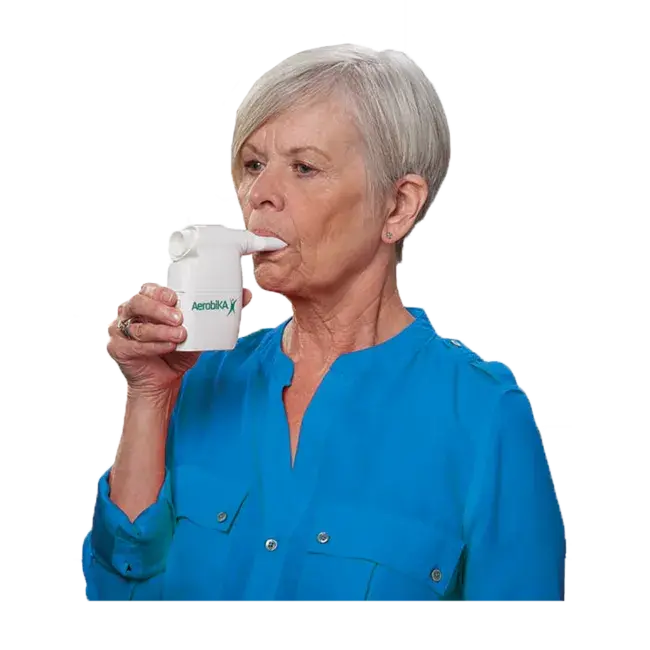
- Oscillating positive expiratory pressure (OPEP) therapy11,18
An OPEP device is a handheld device that combines positive expiratory pressure (PEP) with oscillations (or vibrations) to help clear secretions from your airways. As you exhale through the mouthpiece, positive pressure holds the airways open and allows air to get behind the mucus. Oscillations help to thin, loosen and move the mucus to the larger airways of your lungs where it can be coughed out.