AIM
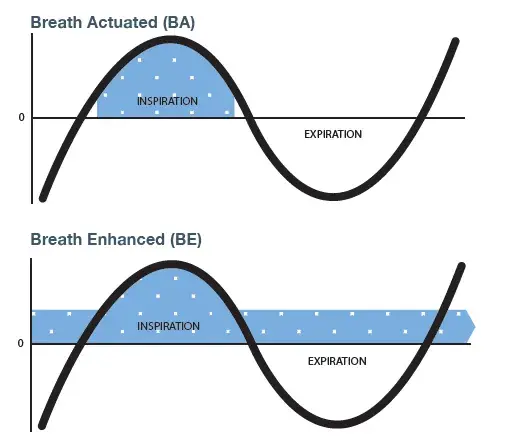
Breath actuated technology (BA) allows for medication delivery to occur only on the inhalation phase of each breathing cycle, whereas breath enhanced technology (BE) delivers aerosol even during exhalation.
We sought to compare the output of two high efficiency nebulizers at different inspiratory:expiratory (I:E) ratios simulating a patient breathing pattern with obstructive lung disease.
METHODS
Each nebulizer/compressor (AeroEclipse* XL BAN* (BA)/Ombra* Table Top (230 Volt) and PARI LC† Sprint (BE)/PARI BOY† Classic) was filled with 2 mL of 1 mg/mL salbutamol sulphate and the mouthpiece connected to a breathing simulator (ASL 5000).
Tidal volume was fixed at 500 mL, but I:E ratio and rate/minute (BPM) were varied (see Graph). Aerosol was collected at minute intervals and drug recovered from the filter assayed by HPLC. That mass was multiplied by fine droplet fraction (%<4.7μm) measured via Spraytec laser diffractometer to calculate fine droplet mass (FDM).

RESULTS
Measures of FDM (μg; mean ± SD) are summarized in the graph below. FDM from the BA nebulizer was unaffected by changes in breathing pattern, whereas output from the BE nebulizer was lower and decreased with increasing I:E ratio.
CONCLUSION
More consistent dose delivery was achieved with the breath actuated technology rather than breath enhanced.
Delivering medication only when the patient inhales would result in more stable therapy if I:E ratio was to change with disease progression or if the patient took breaks to talk during treatment.
MD-301A-0623 * trade marks and registered trade marks of Trudell Medical International (TMI). † trade marks of their respective companies. ©TMI 2023.
