INTRODUCTION
Post-operative pulmonary complications (PPCs) are a variety of conditions adversely affecting the respiratory system after anesthesia and surgery.
Strategies to prevent and treat PPCs include techniques of lung re-expansion using incentive spirometry (IS), which is typically standard of care in the US, and oscillating positive expiratory pressure (OPEP) devices.
However, recent systematic reviews concluded that there is a lack of evidence regarding the effectiveness of IS for the prevention of PPCs in cardiac, thoracic, or upper abdominal surgery.
Previous studies have shown that the addition of an OPEP device to standard of care (IS) reduced all cause rehospitalizations and mean length of stay.1
This real-world retrospective study aimed to assess usage patterns of IS vs an OPEP device, and the impact on post-surgery PPCs.

METHODS
Adults ≥18 years of age with ≥1 hospitalization for cardiac, thoracic or upper abdominal surgery between 9/1/2013 and 7/1/2021 were identified from IQVIA’s Hospital Charge Detail Master (CDM) database and linked to IQVIA’s prescription (LRx) and medical claims (Dx); index visit was the first hospitalization for surgery.
The IS only cohort included patients who had ≥1 CDM, Dx, and LRx record within 12 months prior to index visit and ≥1 CDM and Dx record after discharge, evidence of IS use and one surgery type during index hospitalization, and no evidence of any PEP or OPEP any time during or up to 3 months before index visit.
The OPEP only cohort was selected similarly, except that patients were required to have evidence of a specific OPEP device (Aerobika*, Monaghan Medical) use during index hospitalization and no evidence of IS, OPEP, or PEP use up to 3 months before index visit.
OPEP patients were 1:1 matched to IS patients using propensity score (PS) matching on age, gender, region, payer type, surgical procedure, index year, baseline comorbidity profile, and index visit duration.
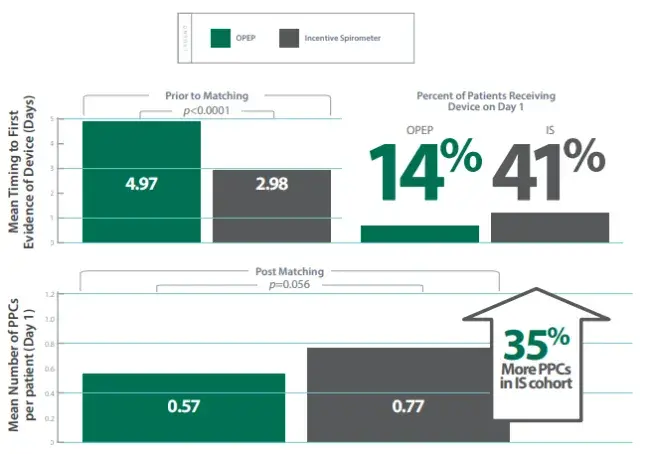
The timing of the device introduction during the index visit was assessed, as were the incidence of PPCs during the visit.
RESULTS
CONCLUSION
This real-world study highlights that current US hospital practice favors the introduction of IS earlier than OPEP for post operative care.
- The hypothesis being that OPEP is given more commonly as a reactive measure to observed complications.
When matched patient groups were compared, there was a trend towards less PPCs for the Aerobika* OPEP vs IS if each device was given on day 1. There was a significant increase in PPCs if the introduction of the OPEP device was delayed to day 3 or later.
This study suggests that there could be benefits if the OPEP device was provided earlier and instead of IS when managing post operative care.
